Beyond Compliance: Implementing the CMS THA/TKA PRO-PM and Strengthening Performance Intelligence in ASCs

Authored by Matt Obenhaus, SVP of Design & Engineering and Matt Wilkinson, Manager of Operations & Strategic Growth
Executive Summary
The Centers for Medicare and Medicaid Services (CMS) recently expanded the Ambulatory Surgery Center Quality Reporting (ASCQR) Program to include the patient-reported outcome–based performance measure (PRO-PM) for total hip and knee arthroplasty (THA/TKA), adding a new dimension to how outpatient surgical performance is assessed. For ambulatory surgery centers (ASCs) performing these procedures, the policy requires the collection and submission of patient-reported outcomes data on pain and function before and after surgery through standardized patient-reported outcome measures (PROMs). This represents an incremental but important evolution in ASC quality measurement, extending evaluation beyond procedural processes and safety metrics to include patient-reported improvement over time.
The immediate operational impact of this policy for ASCs is the need to establish reliable PROMs workflows that meet CMS requirements, including defined collection windows, standardized surveying, and data-completeness thresholds. Failure to meet these requirements will carry financial penalties to annual payment updates, making patient-reported outcome–based performance measurement a standing component of ASC quality reporting versus a temporary or optional initiative.
Beyond compliance, PROMs introduce a type of data that differs from most information ASCs currently report. Patient-reported outcomes are longitudinal, typically collected outside the facility, and dependent on patient engagement and follow-up. Incorporating this data alongside existing clinical, operational, and financial information requires coordination across systems and teams, highlighting limitations in traditional reporting resources.
This white paper explores how patient-reported outcomes can be incorporated into a broader business intelligence framework rather than managed as an isolated reporting task. When outcomes data are connected with operational and financial data, ASCs can better understand performance trends, assess variation in patient care, and support more informed operational planning, while still meeting regulatory expectations.
NueHealth supports ASCs in meeting CMS PROMs requirements and in integrating patient-reported outcomes into a purpose-built business intelligence environment. This approach allows ASCs to address current reporting obligations while strengthening the data infrastructure needed for ongoing performance management.
Introduction: The Next Stage of CMS Compliance
CMS recently finalized the expansion of quality measurement in the outpatient setting by incorporating the THA/TKA PRO-PM into the ASCQR Program. The measure evaluates patients' improvement in their self-reported symptoms and functional status after primary elective joint replacement. ASCs performing eligible THA and TKA procedures for Medicare fee-for-service beneficiaries must collect patient-reported outcomes data at two specified time points: preoperatively within 90 days of surgery and postoperatively between 300 and 425 days after the procedure. Administrative claims data, risk variable data, and Medicare enrollment and beneficiary data collection are also required at different points in the patient’s care.
The policy establishes a phased implementation timeline: voluntary reporting period began in 2025, and mandatory reporting begins for procedures performed in calendar year 2028. To comply, ASCs must have the systems and processes in place to submit complete, matched data for at least 45 percent of eligible cases or risk a reduction to their annual payment update (APU) in 2031. Compliance is not optional; how ASCs operationalize PROMs will have implications beyond regulatory adherence, including their ability to adapt to future value-based care models.
Why PROMs Challenge Traditional ASC Operating Structures
While PROMs are not inherently complex, they expose structural limitations in how many ASCs are organized to capture, manage, and report data over time. Traditional ASC quality measures are largely transactional in nature, focusing on whether specific processes or safety requirements were completed. PROMs introduce a different expectation: the ability to demonstrate patient-reported improvement in pain and function over an extended period using longitudinal data.
Moreover, the CMS THA/TKA PRO-PM is being introduced into an operating environment already under pressure. Today's ASCs face a markedly different reality than in previous decades, managing increasingly complex case mixes with higher-acuity procedures that demand greater clinical coordination. At the same time, persistent labor constraints, particularly in nursing and anesthesia, drive wage inflation, scheduling gaps, and the need for enhanced operational workflows. Volatile supply and implant costs further complicate cost control and margin management, leaving little tolerance for inefficiency.
Despite these challenges, many ASCs continue to rely on fragmented data structures. Electronic medical records, practice management, supply chain, revenue cycle, and survey systems often function independently, with limited interoperability. Performance monitoring is frequently dependent on static, retrospective reports that require manual reconciliation across departments — an approach that is poorly suited to longitudinal measurement.
CMS THA/TKA PRO-PM requirements bring these limitations into focus in several ways:
- Extended patient engagement: PROMs collection occurs long after discharge, when patients are often no longer interacting directly with the facility. Engagement gaps lead to missing survey data and potential payment exposure.
- Cross-system data integration: PROMs must be linked to procedural details, patient demographics, and risk-adjustment data that often resides across multiple systems. Manual reconciliation increases administrative burden and the potential for error.
- Comparative visibility: The THA/TKA PRO-PM applies a risk-adjusted, standardized framework that allows outcomes to be compared across ASC, HOPD, and inpatient settings, increasing the importance of data completeness, consistency, and credibility.
Addressing these challenges through manual workflows or narrow point solutions may support initial compliance but lacks scalability. Over time, PROMs risk becoming a persistent operational burden rather than a source of meaningful insight. More importantly, framing PROMs solely as a quality reporting requirement understates their significance. In practice, patient-reported outcomes are critical performance metrics.
Forward-looking ASC leaders recognize the CMS THA/TKA PRO-PM mandate as more than a compliance exercise. Instead, they view it as an entry point to more disciplined data integration that extends beyond reporting to support long-term adaptability in a value-oriented care environment.
NueHealth’s Integrated PROMs and Business Intelligence Solution for ASCs
NueHealth helps ASCs meet the CMS THA/TKA PRO-PM requirement while intentionally integrating patient-reported outcomes into a broader operational, clinical, and financial analytics infrastructure. This approach allows patient-reported outcomes to be addressed within the context of how performance is measured and managed across the ASC, rather than treated as a standalone reporting obligation.
At a foundational level, NueHealth supports the operational execution of CMS THA/TKA PRO-PM requirements through a structured, digital platform designed to support the full lifecycle of data collection and submission. This includes centralized documentation of required patient-reported data within defined preoperative and postoperative timeframes, automated reminders that guide consistent patient follow-up, and built it criteria to meet CMS data-completeness thresholds and submission requirements. Standardized workflows streamline data capture and reduce reliance on manual, staff-intensive processes that are prone to error, helping ASCs exceed regulatory expectations in a reliable and sustainable manner without introducing unnecessary administrative burden.
Once PROMs execution is established, ASCs are positioned to extend their focus beyond compliance to comprehensive performance management. NueHealth’s Insights business intelligence solution is designed to address a more expansive need: helping ASC leaders understand, monitor, and improve performance across all domains.
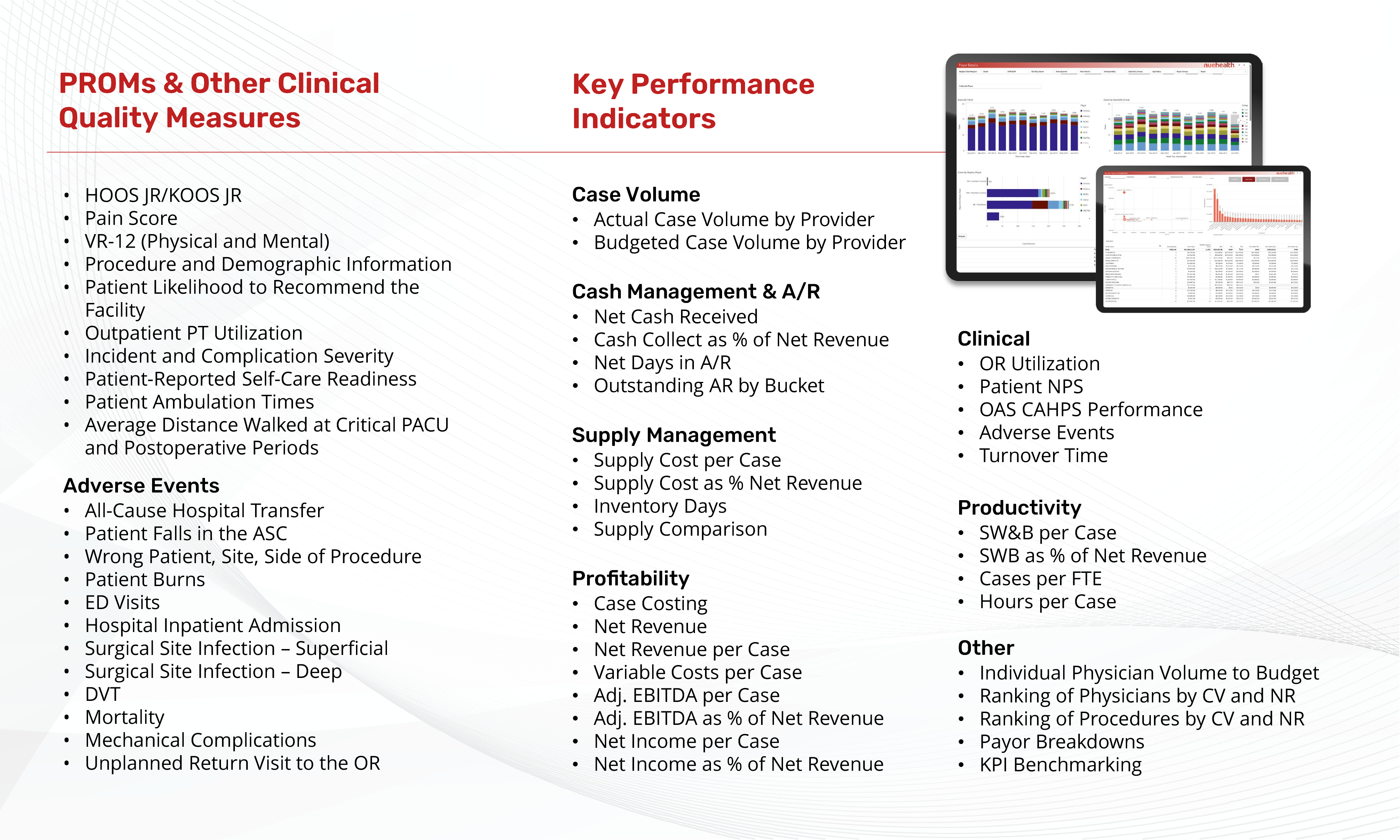
Through the Insights platform, data across ASC source systems are consolidated into a normalized and governed analytics environment that serves as a single foundation for performance evaluation. Within this environment, ASC leaders can visualize and assess operational, clinical, and financial performance across hundreds of metrics, such as case-level margins, block and operating room utilization, and payor mix. Patient-reported outcomes represent one dataset within this wider framework, contributing longitudinal outcomes context alongside other key performance indicators (KPIs). A representative subset of these KPIs, PROMs, and other clinical quality measures is included in the following table:
This enterprise business intelligence solution allows ASC leaders to move beyond retrospective reporting and toward ongoing performance visualization, monitoring, and granular analysis. Interactive dashboards and custom reports support trend analysis over time, comparison across service lines and physicians, and earlier identification of variation or inefficiencies that may warrant intervention.
A key capability of NueHealth’s solution is its ability to produce complex, cross-functional performance metrics that reflect how ASCs generate value in practice. One example is profitability per OR minute — a composite metric incorporating key aspects of what drives bottom line: OR efficiency, block schedule management, case-level costing, and reimbursement. Producing metrics of this complexity requires disciplined data capture across departments, including detailed implant and supply tracking at the case level, as well as consistent integration between EMR and financial systems.
By enabling this level of analytic depth for ASCs, NueHealth supports meaningful benchmarking across facilities, service lines, physicians, payors, and procedure types. ASC leaders gain actionable insight into where performance differs, what is driving that variation, and how operational decisions, financial outcomes, and patient-reported results intersect over time.
Taken together, NueHealth’s approach helps ASCs exceed CMS THA/TKA PRO-PM requirements, while also implementing a more comprehensive business intelligence solution for leaders seeking deeper visibility into performance and greater control over increasingly complex operations.
Laying the Groundwork for the Future of Analytics and AI
As healthcare organizations explore artificial intelligence (AI), a common misconception is that value comes from algorithms alone, when in reality, AI amplifies the quality of the foundational data it processes. In fragmented, inconsistent data environments, AI magnifies noise; in well-governed settings, it accelerates insights. The Healthcare Information and Management Systems Society (HIMSS) AI Task Force notes that “organizations that prioritize data governance and interoperability before deploying AI experience higher adoption and lower long-term risk.”
NueHealth’s approach to AI emphasizes foundational elements. Data must be mapped and unified before advanced analytics can deliver meaningful value. Properly integrated PROMs collection requirements strengthen that foundation rather than complicating it.
Within NueHealth’s platform, AI is applied in practical, supportive ways that assist clinicians and operators rather than replace judgment or workflow ownership. These capabilities include accelerating data reconciliation, identifying outliers and anomalies, surfacing trends across large datasets, and reducing the friction associated with performance analysis and reporting. Because PROMs data is structured, standardized, and collected over time, it is particularly well suited for use in predictive and pattern-recognition models. When combined with broader clinical, operational, and financial data, patient-reported outcomes can contribute to earlier signal detection and more informed performance monitoring.
By investing in strong data discipline and the right supporting tools, ASCs are better positioned to adopt AI responsibly without introducing new sources of risk or undermining confidence in their data.
Conclusion: Owning the Outcomes
Market and regulatory forces are converging in ways that create compelling economic and compliance-driven reasons for ASCs to invest meaningfully in technologies focused on patient-reported outcomes data capture and analysis, outcomes management, and enterprise business intelligence.
Rising labor, supply, and anesthesia costs, combined with payor reimbursement rates that are not keeping pace, are placing increasing pressure on ASC margins. These market forces and dynamics create a clear imperative to manage payor and case mix more deliberately, improve operating room efficiency, and exercise greater discipline around cost management. At the same time, the highest-performing ASCs are sought after for acquisitions or joint venture partnerships by private equity firms and health systems. ASCs that fail to manage these forces through modern technologies and robust business intelligence strategies will experience operational strain and miss potential opportunities for significant equity gains.
Beyond market pressures, the compliance obligations associated with collecting, managing, and reporting total joint arthroplasty patient-reported outcomes further elevate the importance of these investments. In the absence of a technology-enabled strategy, ASCs must resort to burdensome manual processes that are costly and prone to clinical and clerical errors that degrade the provider and patient experience, reduce Medicare payments, and ultimately undermine patient outcomes.
NueHealth has invested in and implemented these strategies for ASC clients for more than a decade and continues to expand adoption beyond the “early-innovator” phase. A foundational component of this approach is the layering of core technologies such as digital EMRs, practice management systems, supply chain, and financial management systems, followed by integrated business intelligence that provides a comprehensive understanding of the ASC’s operating environment and enable action based on that insight.
With this foundation in place, ASCs are better positioned to manage increasing procedural complexity, including total joint and spine cases, across the patient care journey and prepare to meet CMS THA/TKA PRO-PM requirements as the mandate takes effect. The critical next step for ASC leaders is to begin establishing and implementing these strategies in 2026, well ahead of mandatory reporting timelines.
For ASC leaders and physicians seeking a credible, experienced partner across these domains, NueHealth stands ready to collaborate in building a strategy that aligns with the specific needs and goals of their ASC. Contact our team to learn more and schedule a demo.



